| Home Page |
General ANS Features |
Sympathetic Division |
Parasympathetic Division |
Trace Pathways |
Physiology & Pharmacology |
Most-specifically, the term Autonomic Nervous System (ANS) refers to efferent two-neuron pathways that innervate smooth muscle, cardiac muscle & glands. Most-generally, ANS includes both afferent & efferent visceral innervation, as well as the Central Nervous System (CNS) structures that control visceral innervation. Visceral organs vary in their dependence on CNS neural control (e.g., enteric function is least dependent whereas micturition is highly dependent on the CNS). For a presentation of CNS components associated with visceral innervation click here: CNS Control.
 Sympathetic and Parasympathetic divisions of the ANS differ functionally. The parasympathetic division, which innervates viscera in body cavities plus genitalia and head viscera, functions to restore routine visceral status and implement specific visceral functions. The sympathetic division, which innervates viscera throughout the body, also has routine functions (e.g., maintaining normal blood pressure), but its most dramatic role is to prepare for energy intensive "fight or flight" by mobilizing a global visceral response. Click the above image to view the Innervation Table.
Sympathetic and Parasympathetic divisions of the ANS differ functionally. The parasympathetic division, which innervates viscera in body cavities plus genitalia and head viscera, functions to restore routine visceral status and implement specific visceral functions. The sympathetic division, which innervates viscera throughout the body, also has routine functions (e.g., maintaining normal blood pressure), but its most dramatic role is to prepare for energy intensive "fight or flight" by mobilizing a global visceral response. Click the above image to view the Innervation Table.
Autonomic preganglionic neurons synapse on postganglionic neurons. The preganglionic neurons release acetycholine (ACh) which binds to nicotinic receptors (nAChR) on postganglionic neurons. The nicotinic receptors are cation channels; when open, they enable depolarization (excitation) of postganglionic neurons.
Autonomic postganglionic neurons release either acetycholine (ACh) or nor-epinephrine (NE), the former neurons are designated cholinergic, the latter adrenergic. All parasympathetic postganglionic neurons are cholinergic. The great majority of sympathetic postganglionic neurons are adrenergic (except that neurons innervating sweat glands, arrector pilli muscles, and some vessels are cholinergic). Cells of the adrenal medulla, which are modified postganglionic neurons, release mainly epinephrine (adrenalin).
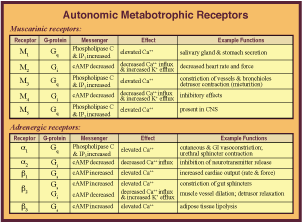 Both ACh and NE can bind to several different types of receptors. All of the receptors are metabotrophic and coupled to G proteins that amplify the neural effect via second messengers. There are five types of muscarinic receptors (mAChR) to which ACh binds. Receptors M1, M3 & M5 involve Gq proteins that elevate C++, resulting in smooth muscle contraction and gland secretion. Receptors M2 & M4 involve Gi proteins that decrease cAMP and have inhibitory effects (M2 decreases heart rate). Click the image on the left to view the Receptor Table enlarged.
Both ACh and NE can bind to several different types of receptors. All of the receptors are metabotrophic and coupled to G proteins that amplify the neural effect via second messengers. There are five types of muscarinic receptors (mAChR) to which ACh binds. Receptors M1, M3 & M5 involve Gq proteins that elevate C++, resulting in smooth muscle contraction and gland secretion. Receptors M2 & M4 involve Gi proteins that decrease cAMP and have inhibitory effects (M2 decreases heart rate). Click the image on the left to view the Receptor Table enlarged.
The two major categories of adrenergic receptors (AR) are designated alpha and beta. Each has sub types: Receptor α1 involves a Gq protein that elevates C++, resulting in smooth muscle contraction. Receptor α2 involves a Gi protein that decreases cAMP and C++ influx which inhibits neurotransmission. Receptors β1, β2 & β3 involve a Gs protein and cAMP elevation that increases C++ for smooth muscle contraction (β2 can be linked to a Gi protein that decreases cAMP resulting in smooth muscle relaxation). Thus the effect of ACh and NE can be either excitory or inhibitory, based on the receptor distribution within visceral organs.
Both ACh and NE are synthesized locally and packaged inside synaptic vesicles located within varicosities (enlargements) found on terminal branches of postganglionic neurons.  Ca++ influx during postganglionic terminal branch depolarization enables synaptic vesicles to merge with the plasma membrane and release ACh (or NE) by exocytosis. The released transmitter molecules diffuse and bind to membrane receptors, triggering G protein dissociation. In the case of ACh, receptor activation is stopped by enzymatic degradation (degradation products are transported into nerve terminals and recycled). NE activity is stopped by neuronal uptake of the intact transmitter molecules, for subsequent degradation or recycling. Click the image on the right to view synapstic vessicles enlarged.
Ca++ influx during postganglionic terminal branch depolarization enables synaptic vesicles to merge with the plasma membrane and release ACh (or NE) by exocytosis. The released transmitter molecules diffuse and bind to membrane receptors, triggering G protein dissociation. In the case of ACh, receptor activation is stopped by enzymatic degradation (degradation products are transported into nerve terminals and recycled). NE activity is stopped by neuronal uptake of the intact transmitter molecules, for subsequent degradation or recycling. Click the image on the right to view synapstic vessicles enlarged.
